Claims management is the heart of every insurance operation—but let’s face it, the traditional system is outdated. Think hours wasted on manual data entry, delays in payouts, frustrated customers, and a process so paper-heavy it feels like it belongs in the last century. It’s inefficient, error-prone, and expensive to maintain. Now, imagine a system where claims are processed in minutes, fraud is flagged automatically, and customers receive personalized updates in real-time.
Welcome to the future of claims management, powered by AI-driven automation. At Haystream, we’re not just talking about disruption—we’re delivering it.
The Problems Plaguing Claims Management Today
Before we dive into the solution, let’s confront the elephant in the room: the challenges that bog down insurers. Here’s what’s broken:
- Manual Processes: Despite technological advancements, 40% of insurance carriers still rely on manual data entry for claims processing, leaving sufficient room for automation of administrative tasks.
- High Error Rates: Manual workflows are prone to errors, with the average insurer spending 30-40% of their time on rework due to inaccuracies in data capture.
- Fraud Detection Issues: Fraudulent claims account for an estimated 10% of all insurance payouts in the U.S., resulting in $40 billion in annual losses.
- Customer Frustration: 52% of policyholders say they would switch insurers after a single bad claims experience.
Sound familiar? These inefficiencies aren’t just operational headaches—they’re hitting insurers where it hurts: revenue, reputation, and customer retention.
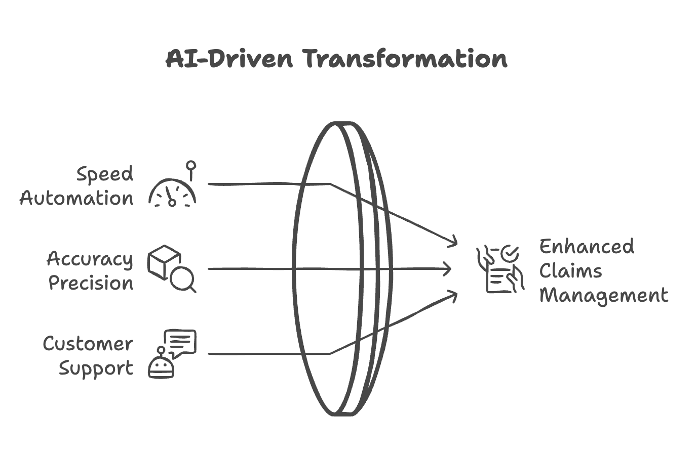
How AI is Changing the Game
AI and automation are rewriting the rulebook for claims management, transforming it from a cumbersome process into a seamless experience. Here’s how:
- Speed Like Never Before
AI-powered automation slashes claims’ processing times from days to minutes. Tools like Natural Language Processing (NLP) extract critical data from unstructured sources—emails, handwritten forms, even social media—while computer vision assesses damage from images in seconds.
- Accuracy That Builds Trust
By removing human error, AI ensures claims data is captured and validated with precision. Fraud detection algorithms analyze patterns across millions of records to flag suspicious claims before they’re paid.
- Customer-First Approach
AI chatbots and virtual assistants provide 24/7 support, answering policyholder questions and delivering real-time updates. Sentiment analysis tools ensure you’re not just resolving claims but delighting customers at every step.
 Real World examples from other Insurance Players Revolution
Real World examples from other Insurance Players Revolution
Across the globe, insurers are leveraging advanced technologies like AI, blockchain, and IoT to redefine claims management and improve operational efficiency. Here are some notable examples of digital transformation in action:
1. Allstate’s Telematics Innovation
Allstate has been a pioneer in adopting telematics through its Drivewise program, which uses real-time driving data to assess risk and offer usage-based insurance (UBI). This initiative has not only improved risk accuracy but also incentivized safer driving behaviors, leading to a reduction in claims costs while enhancing customer satisfaction.
2. Lemonade’s AI-Powered Claims System
Lemonade, a disruptor in the insurance industry, uses AI bots to handle claims. Its system resolves 30% of claims in seconds without human involvement. This rapid resolution improves customer experiences while keeping operational costs low. The company’s AI-driven fraud detection has also minimized financial leakage.
3. AXA’s Blockchain Integration
AXA introduced Fizzy, a blockchain-based insurance product for flight delays. The platform automates claims processes by triggering payouts immediately when flight delay criteria are met. This eliminates manual intervention, reduces processing time, and enhances customer trust by ensuring transparency.
4. State Farm’s AI Claims Processing
State Farm uses computer vision and predictive analytics to automate damage assessment in auto insurance claims. By analyzing photos of vehicle damage, the company has significantly reduced claims processing times, enabling faster settlements for policyholders.
These examples highlight the transformative potential of technology in reshaping the insurance landscape. Companies that embrace digital transformation not only streamline their operations but also elevate customer experiences, setting benchmarks for the industry.
Tools Driving the Transformation: AI for a Purpose
The technology driving this revolution includes:
- Contextualized Machine Learning and Natural Language Processing (NLP): Extracts data from documents to speed up claims’ intake. Such an approach far outperforms most so-called Intelligent Document Processing (IDP) and other enhanced OCR applications that are commonly used today for automating these processes. These techniques, customized to insurers’ specific business, also significantly enhance monitoring for potential fraud.
- Computer Vision: Automates damage assessment by analyzing photos and videos.
- Predictive Analytics: Identifies patterns to prevent fraud and predict claim outcomes.
- IoT Integration: Leverages real-time data from smart devices and telematics for more accurate assessments.
Haystream’s approach, which focuses on delivering business outcomes, applies the right AI methods that are fit for purpose for solving targeted problems. Not everything requires an advanced AI model, and this approach ensures using the right methods, such as traditional BI dashboards, smart genAI-driven chatbots, advanced data visualization models, and embedded smart AI-driven analytics.
Achieving The Dream Team of Claims Automation
Haystream’s AI Jumpstart and Proof of Value (PoV) programs are designed to help insurers adopt AI quickly, with measurable ROI. In just 6–8 weeks, we deliver outcomes like faster claims resolutions, reduced operational costs, and improved customer satisfaction by focusing their data preparation and management efforts for specific use cases.
Paired with using the right analytics, insurers gain a holistic view of claims data, empowering smarter decisions and uncovering hidden opportunities. Together, we bring the tools and expertise needed to modernize claims management for the digital age.